What Is Ta Similar Dermatological Skin Disease Related To Dhoenbergs?
- Research article
- Open Access
- Published:
The psychosocial adaptation of patients with skin disease: a scoping review
BMC Public Health volume 19, Article number:1404 (2019) Cite this article
Abstract
Background
Skin illness is a global public health trouble that ofttimes has physiological, psychological and social impacts. Even so, it is non very clear how to adapt to these impacts, especially psychosocial accommodation of patients with skin disease.
Methods
We searched EMBASE, PubMed, CINAHL and PsycINFO from 2009 to 2018. The following themes were extracted from the included articles: the concepts, related factors, and interventions for psychosocial adaptation of patients with peel illness. Two reviewers independently screened and analyzed.
Results
From 2261 initial records, 69 studies were identified and analyzed. The concept of psychosocial adaptation in patients with pare disease was referred to under an array of descriptions. The related factors for psychosocial accommodation in patients with skin disease included the following: demographic factors (sex activity, historic period, education level, ethnicity, BMI, sleep quality, marital status, practice amount, family history, the employ of topical handling only, personality and history of smoking); illness-related factors (disease severity, clinical symptoms, localization and duration); psychological factors (anxiety/depression, self-esteem, body prototype, stigma and suicidal ideation); and social factors (social support, social interaction, sexual life, economical burden and social acceptance). Despite being limited in quantity, several studies take clarified the benefits of adjuvant care in the form of cognitive behavioral training, educational training and self-help programs, all of which have get common methods for dealing with the psychosocial impacts.
Conclusions
Based on the previous literatures, we constructed a protocol of care model for psychosocial adaptation in patients with skin illness. It not just provided the direction for developing new instruments that could assess psychosocial accommodation statue, but also a basis for helping patients arrange to changes in skin affliction.
Introduction
As the largest organ of the human being body, the skin is the primary bulwark that resists the outside world.one Considering skin diseases are often not life-threatening, attending and funds may be invested in diseases considered more serious. However, the psychosocial and occupational impact of skin illness is ofttimes comparable to, if not greater than, other chronic medical conditions.2 The lifetime prevalence of skin disease was reported from European five countries, with skin disease including eczema (xiv.2%), atopic dermatitis (7.9%), psoriasis (5.2%) and vitiligo (1.9%).3 With the deterioration of environment and various pressures, the incidence of skin disease has increased in recent years. Information technology has get a global public health problem.iv Many skin diseases have a chronic and repeated process, which requires us to care for the disease and assist patients positive accommodation.5
Roy defines adaptation as the process and outcome whereby thinking and feeling persons as individuals or in groups use witting awareness and choice to create human and environmental integration, including physiological, psychological and social aspects.6The British Association of Dermatologists suggested that 85% of patients with peel disease have reported that the psychosocial impacts of their disease are a major component of illness, which is a concerning statistic.7 Psychological and social analyses reveal that if the trunk is stimulated past stress and the external surroundings, the emotional state will change equally an instinctive response.viii Skin disorders can significantly bear on the psyche, and the psyche can significantly affect skin disorders through psycho-neuro-immuno-endocrine and behavioral mechanisms.9 And the stress is related to functional and psychological processes in pare disease patients with loftier levels of anxiety sensitivity.eight In response to the environmental pressures of extreme grief and fear, individuals will experience continuous tension.ten Skin diseases misconstrue body image, which may accept a negative bear upon on the psychosocial health and quality of life (QOL) of patients.11 A loftier severity of itching, pain, and scaling in psoriasis patients is related to loftier disease severity and low QOL and work productivity.12 The psychosocial adjustment to vitiligo is mainly affected past subjective factors.13
Therefore, it volition exist limited to attempts to understand the psychosocial impacts of psoriasis from the perspective of current measurements of demographic characteristics and disease severity.fourteen It is imperative to develop advisable psychosocial adaptation (PA) evaluation tools for patients with skin disease.15 Various dispensary models accept been described to provide specialised psychodermatology intendance in specific settings.16 Notwithstanding, it is not clear the concepts, related factors and interventions of PA for patients with skin diseases. They were described by this scoping review. Based on the previous literatures, we attempted to present a protocol of care model for PA in patients with skin disease.
Methods
A scoping review can examine and clarify broader areas than a systematic review to identify gaps in the evidence, analyze central concepts, and report on the types of evidence that accost and inform practices in the topic expanse.17 Therefore, a scoping review method was chosen to allow for the inclusion of different written report designs; this type of report follows the methodology model proposed by Arksey and O'Malley to map the various concepts underpinning this research area, as well as to clarify the related factors and interventions.xviii We followed the guidelines of the PRISMA-ScR19 which is included as an Boosted file 1 document to this paper. We did non provide detailed critical appraisal of private studies or meta-analyses every bit this is a developing area of research. The steps of the review are outlined beneath.
Identifying the research questions
This scoping review aimed to identify the diverse concepts and related factors of PA for patients with skin affliction past mapping the existing literature in the field to provide a basis for developing instruments to appraise the status of PA. Additionally, mapping showed a diverseness of interventions.
Identifying relevant studies
The search strategy was formed by the project team and consulting with information specialists (come across Boosted file two). The following databases EMBASE, PubMed, CINAHL and PsycINFO were chosen and searched from 2009 to 2018 for publications with no limit on language, which covered a broad range of subjects including medicine, psychosociology and nursing. EndNote was applied to exclude duplicate records and manage inclusion literatures.
Selecting the literature
The inclusion criteria were as follows:
-
Population: Patients experiencing peel diseases diagnosed as psoriasis, atopic dermatitis, eczema, vitiligo or chronic urticaria.
-
Range of concepts: The psychosocial adaptation of patients in unlike skin weather. Co-ordinate to previous research and squad discussion, the post-obit concepts were often used to reflect psychosocial impacts of patients with skin diseases: anxiety/depression, trunk epitome, stigma, self-esteem, social support, family function, fiscal costs and piece of work. Some studies fifty-fifty equated the PA of patients with the QOL.
-
Context: Adult population for 18 years old or older.
All articles provided master data on the various concepts, related factors and interventions of PA for patients with skin disease from 2009 to 2018. Single case reports and comments were excluded. Firstly, in lodge to avoid missing valuable literature, ii researchers conducted iii rounds of assessments that included reading the study titles and abstracts for the inclusion and exclusion criteria. 2nd, the full texts of the studies identified through screening were independently assessed for eligibility by two authors. Third, the studies were classified for mapping according to the definitions and descriptions of methods provided in the publication.17 Finally, data extraction was undertaken by 1 author (JBI systematic review researcher) using a structured form. The accurateness of information extracted from the included studies was checked by another writer. Any disagreements were resolved by a larger team give-and-take.
Charting the information
A total of 69 articles were finally included in this review and were so subjected to data charting. The data charting took the following information into consideration: writer(s), year of publication, country of origin, study population, sample size, methodology, concept, assessment tool, related factors and interventions of PA for patients with skin diseases.
Collating, summarizing, and reporting the literature
The various concepts of PA for patients with skin diseases were identified. The related factors in the papers reviewed were classified every bit demographic, physiological, psychological or social factors. The interventions were reported.
Results
The search strategy yielded 2261 potential papers. After removing duplications (n = 548) and eliminating 936 by a showtime pass through the titles and abstracts, the potentially relevant literature was screened in two rounds and resulted in 69 studies. The remaining studies were amassed in the following three facets: i) diverse concepts of PA (northward = 7), ii) related factors of PA (n = 51), and three) interventions (due north = 11) (Fig. ane). The characteristics of the included literature are presented in Table 1.
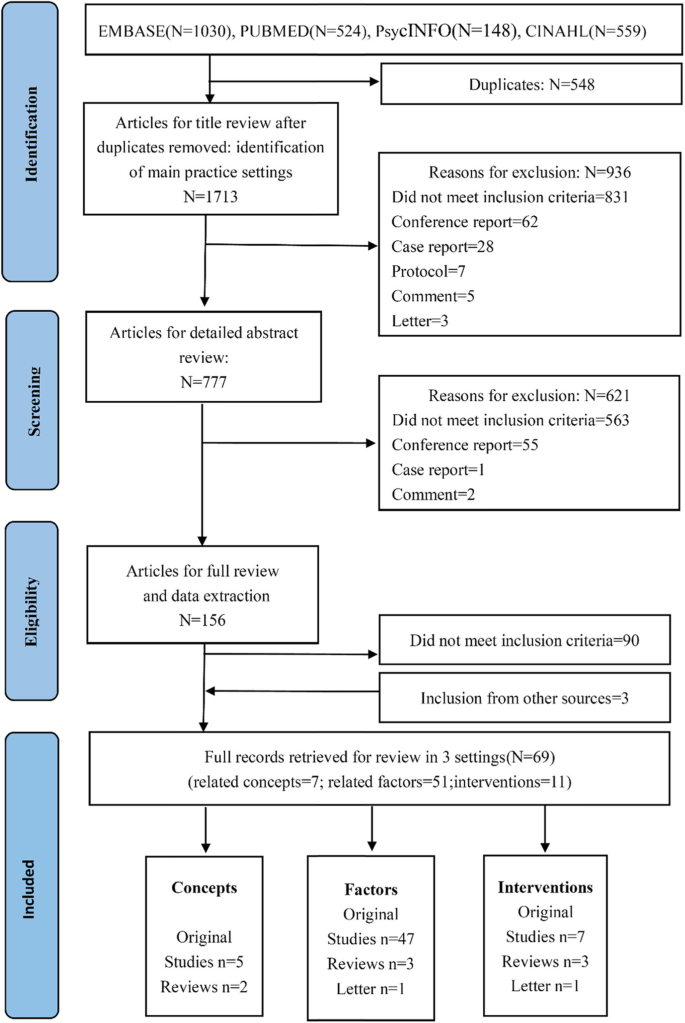
PRISMA menses diagram of illustrating literature search and selection
Various concepts of psychosocial accommodation for patients with skin disease
A clear conceptual definition of psychosocial adaptation is identified past Rodgers' evolutionary concept analysis, and the identified attributes of PA include modify, process, continuity, interaction and influence, all of which were nowadays in the multidisciplinary literature reviewed, thus demonstrating the wide utilize of the concept.20, 21 In the nineteenth century, peel diseases were linked to psychosocial factors. The mechanism was proposed and clarified in subsequent decades, and multidisciplinary collaboration was crucial to promote the adaptation of patients with skin diseases.22 PA was referred to nether an assortment of descriptions in pare diseases including psychosocial factor,11, 23 burden,24, 25 impact,26 morbidity,15 and attribute.27 The measurement methods used in the literature are shown in Table two.
Related factors of psychosocial accommodation for patients with skin affliction
Table three shows the related factors of PA for patients with skin disease including the demographic, illness-related, psychological and social factors.
Demographic factors
With regard to demographic facets, the primal factors reported were sex,13, 28,29,30,31,32,33,34,35,36,37,38 age,31, 35, 38,39,40,41 education level,34, 36, 41,42,43 ethnicity,32, 42 BMI,44, 45 slumber quality,46, 47 marital status,28, 48 practice amount,49 family history,43 the use of topical treatment merely,32 personality13 and history of smoking.44 Females were more prone to depressive and psychosocial maladaptation than males with skin disease.28, 31, 50 Because females were more likely to believe in the importance of physical appearance to their personal or social values than males, their investment in concrete attractiveness was significantly increased. Psychological impacts related to skin disease may largely be attributed to the patients' maladaptive assumptions well-nigh advent and society'southward focus on the perfect body and beauty. However, the genital lesions in males were more prone to cause sexual dysfunction than the lesions in females.35 There was no understanding for the affect of age on psychosocial level.31 Younger psoriasis patients can experience feelings of embarrassment, disturbance of daily activities, poor physical health, and depression productivity at work. Nevertheless, it was as well constitute that old historic period was related to a loftier risk for depression in atopic dermatitis patients. Didactics level also influenced the QOL of patients with psoriasis.
Disease-related factors
The disease-related factors were severity,12, 31,32,33,34, 36, 39,40,41, 43, 49, 51,52,53,54,55,56,57,58,59,60 clinical symptoms (itching,47, 48, 52, 61 pain, scaling),12, 54, 62 localization (visible and genital parts)28, 34, 43, 50, 63, 64 and duration.28, 29, 33, 43 The severity of the pare illness was associated with the level of depression and feet, and it had a negative effect on QOL.23, 27 Itching is the cardinal clinical symptom of patients with pare disease, which tin can result in slumber deprivation and mental disorders. However, the localization of the peel lesions was frequently more than important than the affliction severity and was associated with negative mental health, including low, social feet, self-image disorder, and stigmatization. The 'sensitive' trunk regions were defined as the visible parts of the body, which included the scalp, face, cervix, hand and fingernails.43 Additionally, the psoriasis lesions located on the genitals, buttocks, abdomen, breast or lumbar region were more likely to lead to sexual dysfunction.64 The clinical symptoms of psoriasis, particularly itching, pain and scaling, negatively afflicted health outcomes and work productivity.62
Psychological factors
With respect to psychological facet, the related factors included feet and depression,36, 39, 40, 42, 44,45,46, 48, 55, lx, 61, 65 self-esteem,thirteen, 34, 53, 66 torso image,xxx, 53, 67 stigma29, 41 and suicidal ideation.46, 48 Skin disease patients take a high level of anxiety or depression. Proinflammatory cytokines such as IL-1 and IL-6 were found in both psoriasis and depression, indicating that the inflammatory process may exist involved in the progression of both diseases.68 Depression in psoriasis patients was related to a high risk of stroke and cardiovascular death, especially during acute depression.69 The adaptation of vitiligo patients has been considered to be affected past self-esteem levels. The following five mutual themes of stigma take been identified in patients with psoriasis: anticipation of rejection, feelings of being flawed, sensitivity to the attitudes of society, secretiveness, guilt and shame.15 A high level of stigma and low self-esteem have negative effects on patient compliance.
Social factors
The social factors of PA in patients with skin disease were: social back up,29, 37, 40, 49, 57, 70 social interaction,36, 67, 70, 71 sexual life49, 63 and economic burden 42, 72,73,74,75,76 (medical expenses,52 piece of work productivity,12, 52, 54, 59, 62, 77, 78 income level43, 51). It was plant that high levels of perceived social back up were positively correlated with the depression occurrence of depressive symptoms.11 The marriages and relationships of 50% of vitiligo patients were negatively affected by skin disease.79 Due to its physical symptoms and the stigma caused by the appearance of peel, psoriasis tin can be considered a socially isolating illness.68 Psoriasis, a chronic inflammatory peel affliction, seems to exist related to erectile dysfunction, which was a predictor of hereafter cardiovascular disease.65 It is critical to accurately evaluate constructive treatments of pare disease to understand the interaction between lost productivity, straight costs and quality of life.76
Interventions of psychosocial adaptation for patients with skin disease
The outcomes of PA include positive and negative aspects.20 Tabular array iv shows the PA interventions of skin disease included cerebral behavioral therapy,80,81,82,83,84,85,86 educational training,82, 87,88,89 cocky-aid programs,lxxx, 81, 84 psychotherapy84 and advice.90
Discussion
This scoping review analyzed the contents of 69 papers with results that were iii-fold: i) some reported the various concepts of PA for patients with skin disease, which required that futurity inquiry should unify the terms; ii) some reported the related factors of PA for patients with skin illness, which provided a basis for developing instruments that appraise the status of PA for patients with skin disease; and iii) others reported a variety of interventions, which provided a ground for formulating a protocol of care model for PA in patients with skin disease.
Patients with peel disease frequently accept to cope with a condition that leads to physical disfigurement, psychological destruction and social stigma. Although a large number of studies have been conducted on the treatment of patients with skin diseases, few studies have been directed towards the condition and interventions of the psychosocial adaptation for patients with peel illness. It was shown that psychoeducational intervention for acceptance and managing social touch is needed, which is also the first stride to informing the development of a patient-centered psychological intervention.91 Adding nondrug treatments such equally biofeedback, cognitive behavioral methods, CES, EFT, EMDR, hypnosis, mindfulness meditation, placebo outcome, or suggestions oft enhances the therapeutic effect.ix The major routes for coping with the impacts of peel disease include the doctor-patient relationship, education of the patient and the community about the bodily nature of these diseases, and more structured therapeutic strategies such as private, grouping, or behavioral therapy. In response to patient feedback and Nice guidelines, the 'Psoriasis Direct' service was launched in 2013; this service aims to give patients open up access to specialist nurses when they need it for secondary intendance, and 'Psoriasis Direct' has received overwhelmingly positive feedback.92 Despite being limited in quantity, several studies have clarified the benefits of adjuvant care in the form of cognitive behavioral grooming, educational grooming and self-help programs. An electronic wellness record system for patients with skin disease has not been established for long-term follow-up, and then there is a lack of a systematic care model and financial support.93
Most researchers accept posited models in which accommodation is conceptualized every bit a procedure of change in reaction triggered past functional limitations associated with external environmental antecedents (eg, injury, accidents, traumas) or internal pathogenic condition (eg, disease).21 And the accommodation procedure suggests an unfolding paradigm in which the individual's reactions to his or her chronic illness or disability follow a stable sequence of stage (ie, partially overlapping and nonexclusive psychosocial reactions), or stage (ie, detached and categorically sectional psychosocial reactions) that can be temporally and hierarchically ordered. Others view psychosocial accommodation to chronic illness and disability as one of a gear up of independent and nonsequential patterns of homo behavior.21 Based on previous theories and studies, when individuals accept skin diseases, the individuals will make different primary assessments due to their different demographic, psychological and social conditions. If individuals think they can cope with the skin disease, they will adopt a positive attitude and behavior to face it, which refers to positive psychosocial accommodation. However, if individuals think they cannot cope with the skin disease, they volition endure from psychosocial maladaptation or conduct a secondary assessment. The higher up 2 situations connected to occur after the secondary assessment. If we can carry out targeted psychosocial intervention before the private experience invalid adaptation, nosotros can help patients positively deal with the pare disease then promote patient adaptation (Fig. 2).
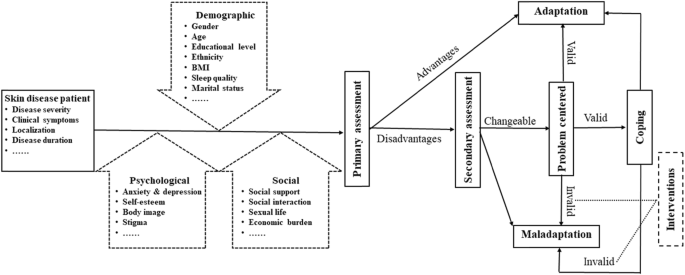
A protocol of care model for psychosocial adaptation in patients with skin disease
Strength and limitations
This research included studies in unlike settings, which brought to light the range of concept and related factors of PA for patients with skin disease, which could provide the management for farther research. A scoping review method was chosen to allow for the inclusion of different study designs, and it does not involve detailed critical appraisal of individual studies or meta-analyses. Considering fractional databases selected and grayness literature not included, the results are used only as an overview of the field.
Conclusion
The clinical process of a series of skin diseases is the consequence of a complex and sometimes reciprocal interaction amidst biological, psychological, and social factors, all of which can play a office in the occurrence and development of skin diseases. This review described the range of concept and related factors of psychosocial accommodation for patients with skin disease, which could contribute to the development of new instruments. The protocol of intendance model based on previous theory and inquiry could provide directions for care and policy that promote psychosocial adaptation for patients with pare disease. Farther inquiry is needed to examine the effectiveness of psychosocial interventions based on the protocol of care model for individuals with peel disease.
Availability of data and materials
All information generated or analysed during this report are included in this published commodity and its supplementary information files.
Abbreviations
- PA:
-
Psychosocial Accommodation
- QOL:
-
Quality of Life
References
-
Basavaraj KH, Navya MA, Rashmi R. Dermatology. United states of america: Elsevier; 2010.
-
Hong J, Koo B, Koo J. The psychosocial and occupational bear upon of chronic peel disease. Dermatol Ther. 2008;21(1):54–9.
-
Svensson A, Ofenloch RF, Bruze M, Naldi 50, Cazzaniga S, Elsner P, Goncalo M, Schuttelaar MA, Diepgen TL. Prevalence of peel illness in a population-based sample of adults from v European countries. Br J Dermatol. 2018;178(5):1111–viii.
-
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Report 2016. Lancet. 2017;390:1211–59.
-
Jafferany M, Pastolero P. Psychiatric and Psychological Touch of Chronic Skin Disease. Prim Care CNS Disord. 2018;20(ii). https://doi.org/10.4088/PCC.17nr02247.
-
Roy C. Extending the Roy adaptation model to come across changing global needs. Nurs Sci Q. 2011;24:345–51.
-
Working Party Written report on Minimum Standards for Pyscho-Dermatology Services 2012. http://world wide web.bad.org.uk/shared/get-file.ashx?itemtype=document&id=1622. Accessed 15 Jan 2015.
-
Dixon LJ, Witcraft SM, McCowan NK, Brodell RT. Stress and skin disease quality of life: the moderating role of feet sensitivity social concerns. Br J Dermatol. 2018;178:951–7.
-
Shenefelt PD. Behavioral and psychotherapeutic interventions in dermatology. The handbook of behavioral medicine, vol. Vols. ane–ii: Wiley-Blackwell; 2014. p. 570–92.
-
Folkman S, Lazarus RS. Coping as a mediator of emotion. J Pers Soc Psychol. 1988;54:466–75.
-
Wojtyna E, Lakuta P, Marcinkiewicz K, Bergler-Czop B, Brzezinska-Wcislo 50. Gender, body image and social support: biopsychosocial deter-minants of low amid patients with psoriasis. Acta Derm Venereol. 2017;97:91–7.
-
Korman NJ, Zhao Y, Pike J, Roberts J, Sullivan E. Increased severity of itching, pain, and scaling in psoriasis patients is associated with increased illness severity, reduced quality of life, and reduced work productivity. Dermatol Online J. 2015;10:21 pii: 13030/qt1x16v3dg.
-
Bonotis Thousand, Pantelis M, Karaoulanis Due south, Katsimaglis C, Papaliaga M, Zafiriou E, et al. Investigation of factors associated with wellness-related quality of life and psychological distress in vitiligo. J Dtsch Dermatol Ges. 2016;14:45–9.
-
Perrott SB, Murray AH, Lowe J, Mathieson CM. The psychosocial touch on of psoriasis: physical severity, quality of life, and stigmatization. Physiol Behav. 2000;70:567–71.
-
Foggin E, Cuddy L, Immature H. Psychosocial morbidity in skin disease. Br J Hosp Med (Lond). 2017;78:C82–6.
-
Zhou S, Mukovozov I, Chan AW. What is known about the Psychodermatology clinic model of care? A systematic scoping review. J Cutan Med Surg. 2018;22(1):44–50.
-
Aromataris Due east, Munn Z. Joanna Briggs found Reviewer'southward manual. Due south Australia: The Joanna Briggs Establish; 2017.
-
Arksey H, O'Malley 50. Scoping studies towards a methodological framework. Int J Soc Res Methodol. 2005;8:nineteen.
-
Tricco Air conditioning, Lillie Due east, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel Due south, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
-
Londono Y, McMillan DE. Psychosocial adaptation: an evolutionary concept analysis exploring a common multidisciplinary language. J Adv Nurs. 2015;71:2504–xix.
-
Livneh H, RF A. Psychosocial adaptation to chronic illness and disability: Marylan d:Aspen publishers; 1997.
-
Chouliara Z, Stephen K, Buchanan P. The importance of psychosocial cess in dermatology: opening Pandora'southward box? Dermatol Nurs. 2017;16(four):30–iv.
-
Li L, Liu P, Li J, Xie HF, Kuang YH, Li J, et al. Psychosocial factors of chronic mitt eczema. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2017;42:179–83.
-
Marron SE, Tomas-Aragones L, Navarro-Lopez J, Gieler U, Kupfer J, Dalgard FJ, et al. The psychosocial burden of hand eczema: data from a European dermatological multicentre study. Contact Dermatitis. 2018;78:406–12.
-
Krishna GS, Ramam Yard, Mehta Chiliad, Sreenivas Five, Sharma VK, Khandpur S. Vitiligo impact scale: an instrument to appraise the psychosocial burden of vitiligo. Indian J Dermatol Venereol Leprol. 2013;79:205–10.
-
Richards HL. The psychosocial bear upon of psoriasis: implications for treatment, ProQuest Information & Learning; 2018.
-
Kouris A, Christodoulou C, Stefanaki C, Livaditis M, Tsatovidou R, Kouskoukis C, et al. Quality of life and psychosocial aspects in Greek patients with psoriasis: a cantankerous-sectional study. An Bras Dermatol. 2015;ninety:841–v.
-
Bidaki R, Majidi Due north, Moghadam Ahmadi A, Bakhshi H, Sadr Mohammadi R, Mostafavi SA, et al. Vitiligo and social acceptance. Clin Cosmet Investig Dermatol. 2018;11:383–vi.
-
Lakuta P, Marcinkiewicz K, Bergler-Czop B, Brzezinska-Wcislo 50. How does stigma affect people with psoriasis? Postepy Dermatol Alergol. 2017;34:36–41.
-
Rosinska M, Rzepa T, Szramka-Pawlak B, Zaba R. Body image and depressive symptoms in person suffering from psoriasis. Psychiatr Pol. 2017;51:1145–52.
-
Nicholas MN, Gooderham MJ. Atopic dermatitis, depression, and Suicidality. J Cutan Med Surg. 2017;21:237–42.
-
Lamb RC, Matcham F, Turner MA, et al. Screening for anxiety and depression in people with psoriasis: a cross-sectional study in a third referral setting. Br J Dermatol. 2017;176(4):1028–34.
-
Lakuta P, Przybyla-Basista H. Toward a better understanding of social feet and depression in psoriasis patients: the role of determinants, mediators, and moderators. J Psychosom Res. 2017;94:32–8.
-
Ayala F, Sampogna F, Romano GV, Merolla R, Guida Yard, Gualberti Thou, et al. The impact of psoriasis on piece of work-related problems: a multicenter cross-exclusive survey. J Eur Acad Dermatol Venereol. 2014;28:1623–32.
-
Chen YJ, Chen CC, Lin MW, Chen TJ, Li CY, Hwang CY, et al. Increased adventure of sexual dysfunction in male patients with psoriasis: A nationwide population- based follow- up report. J Sex activity Med. 2013;x:1212–viii.
-
Sampogna F, Tabolli South, Abeni D. Living with psoriasis: prevalence of shame, anger, worry, and problems in daily activities and social life. Acta Derm Venereol. 2012;92:299–303.
-
Janowski K, Steuden Southward, Pietrzak A, Krasowska D, Kaczmarek 50, Gradus I, et al. Social support and adaptation to the illness in men and women with psoriasis. Curvation Dermatol Res. 2012;304:421–32.
-
Chan MF, Chua TL, Goh BK, Aw CW, Thng TG, Lee SM. Investigating factors associated with depression of vitiligo patients in Singapore. J Clin Nurs. 2012;21:1614–21.
-
Kwan Z, Bell YB, Tan LL, Lim SX, Yong ASW, Ch'ng CC, et al. Determinants of quality of life and psychological status in adults with psoriasis. Curvation Dermatol Res. 2018;310:443–51.
-
Dieris-Hirche J, Gieler U, Petrak F, Milch Westward, Te Wildt B, Dieris B, et al. Suicidal ideation in adult patients with atopic dermatitis: A High german cross-sectional study. Acta Derm Venereol. 2017;97:1189–95.
-
Premkumar R, Kar B, Rajan P, Richard J. Major precipitating factors for stigma amid stigmatized vitiligo and psoriasis patients with brown-black peel shades. Indian J Dermatol Venereol Leprol. 2013;79(5):703–5.
-
Kwan Z, Bell YB, Tan LL, Lim SX, Yong As, Ch'ng CC, et al. Socioeconomic and sociocultural determinants of psychological distress and quality of life among patients with psoriasis in a selected multi-ethnic Malaysian population. Psychol Health Med. 2017;22:184–95.
-
Alpsoy E, Polat 1000, FettahlioGlu-Karaman B, Karadag AS, Kartal-Durmazlar P, YalCın B, et al. Internalized stigma in psoriasis: A multicenter written report. J Dermatol. 2017;44:885–91.
-
Molina-Leyva A, Molina-Leyva I, Almodovar-Real A, Ruiz-Carrascosa JC, Naranjo-Sintes R, Jimenez-Moleon JJ. Prevalence and associated factors of erectile dysfunction in patients with moderate to severe psoriasis and healthy population: A comparative study considering physical and psychological factors. Arch Sex Behav. 2016;45:2047–55.
-
Innamorati M, Quinto RM, Imperatori C, Lora V, Graceffa D, Fabbricatore Grand, Lester D, Contardi A, Bonifati C. Health-related quality of life and its association with alexithymia and difficulties in emotion regulation in patients with psoriasis. Compr Psychiatry. 2016;lxx:200–eight.
-
Lee Due south, Xie L, Wang Y, Vaidya North, Baser O. Evaluating the effect of treatment persistence the economic Burden of moderate to severe psoriasis and/or psoriatic arthritis patients in the U.Southward. Department of Defense population. J Manag Care Spec Pharm. 2018;24:654–63.
-
Kimball AB, Edson-Heredia East, Zhu B, Guo J, Maeda-Chubachi T, Shen Due west, Bianchi MT. Understanding the relationship between pruritus severity and piece of work productivity in patients with moderate-to-severe psoriasis: slumber issues are a mediating factor. J Drugs Dermatol. 2016;fifteen(2):183–8.
-
Ahmed AE, Al-Dahmash AM, Al-Boqami QT, Al-Tebainawi YF. Depression, anxiety and stress among Saudi Arabian dermatology patients: cross-sectional study. Sultan Qaboos Univ Med J. 2016;xvi:e217–23.
-
Khoury LR, Danielsen PL, Skiveren J. Body prototype altered by psoriasis. A study based on individual interviews and a model for body image. J Dermatolog Care for. 2014;25:2–7.
-
Lakuta P, Marcinkiewicz K, Bergler-Czop B, Brzezinska-Wcislo L, Slomian A. Associations between site of pare lesions and depression, social anxiety, body-related emotions and feelings of stigmatization in psoriasis patients. Postepy Dermatol Alergol. 2018;35:60–6.
-
Nayak PB, Girisha BS, Noronha TM. Correlation between affliction severity, family unit income, and quality of life in psoriasis: A study from South India. Indian Dermatol Online J. 2018;9:165–9.
-
Hebert AA, Stingl G, Ho LK, Lynde C, Cappelleri JC, Tallman AM, Zielinski MA, Frajzyngier V, Gerber RA. Patient touch and economic burden of mild-to-moderate atopic dermatitis. Curr Med Res Opin. 2018;34(12):2177–85.
-
Nazik H, Nazik S, Gul FC. Body paradigm, self-esteem, and quality of life in patients with psoriasis. Indian Dermatol Online J. 2017;eight:343–6.
-
Korman NJ, Zhao Y, Motorway J, Roberts J. Relationship between psoriasis severity, clinical symptoms, quality of life and piece of work productivity among patients in the The states. Clin Exp Dermatol. 2016;41:514–21.
-
Tee SI, Lim ZV, Theng CT, Chan KL, Giam YC. A prospective cantankerous-exclusive study of anxiety and depression in patients with psoriasis in Singapore. J Eur Acad Dermatol Venereol. 2016;30:1159–64.
-
Yano C, Saeki H, Ishiji T, Ishiuji Y, Sato J, Tofuku Y, et al. Bear upon of disease severity on work productivity and activity impairment in Japanese patients with atopic dermatitis. J Dermatol. 2013;40:736–ix.
-
Schneider K, Heuft G, Hockmann J. Determinants of social anxiety and social avoidance in psoriasis outpatients. J Eur Acad Dermatol Venereol. 2013;27:383–6.
-
Geale Yard, Henriksson Thousand, Schmitt-Egenolf M. How is illness severity associated with quality of life in psoriasis patients? Prove from a longitudinal population-based written report in Sweden. Wellness Qual Life Outcomes. 2017;fifteen(ane):151.
-
Korman NJ, Zhao Y, Roberts J, Pike J, Sullivan E, Tsang Y, Karagiannis T. Touch on of psoriasis flare and remission on quality of life and piece of work productivity: a real-world study in the U.s.a.. Dermatol Online J. 2016;22:7.
-
Pereira MG, Brito Fifty, Smith T. Dyadic adjustment, family coping, torso image, quality of life and psychological morbidity in patients with psoriasis and their partners. Int J Behav Med. 2012;19(3):260–9.
-
Chrostowska-Plak D, Reich A, Szepietowski JC. Relationship betwixt itch and psychological status of patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2013;27:e239–42.
-
Lewis-Beck C, Abouzaid Southward, Xie Fifty, Baser O, Kim Eastward. Assay of the relationship between psoriasis symptom severity and quality of life, work productivity, and activity damage among patients with moderate-to-severe psoriasis using structural equation modeling. Patient Adopt Adherence. 2013;7:199–205.
-
Sarhan D, Mohammed GFA, Gomaa AHA, Eyada MMK. Female genital dialogues: female genital cocky-image, sexual dysfunction, and quality of life in patients with vitiligo with and without genital affection. J Sex Marital Ther. 2016;42:267–6.
-
Molina-Leyva A, Almodovar-Real A, Ruiz-Carrascosa JC, Naranjo-Sintes R, Serrano-Ortega Due south, Jimenez-Moleon JJ. Distribution pattern of psoriasis affects sexual function in moderate to severe psoriasis: A prospective case serial study. J Sex Med. 2014;xi:2882–9.
-
Ji S, Zang Z, Ma H, et al. Erectile dysfunction in patients with plaque psoriasis: the relation of depression and cardiovascular factors. Int J Impot Res. 2016;28:96–100.
-
Ahmed A, Shah R, Papadopoulos Fifty, Bewley A. An ethnographic study into the psychological impact and adaptive mechanisms of living with hand eczema. Clin Exp Dermatol. 2015;40:495–501.
-
Brito Fifty, da Graça Pereira M. Individual and family variables in psoriasis: A report with patients and partners. Psicologia: Teoria e Pesquisa. 2012;28:171–9.
-
Koo J, Marangell LB, Nakamura M, Armstrong A, Jeon C, Bhutani T, et al. Depression and suicidality in psoriasis: review of the literature including the cytokine theory of depression. J Eur Acad Dermatol Venereol. 2017;31:1999–2009.
-
Egeberg A, Khalid U, Gislason GH, Mallbris Fifty, Skov 50, Hansen PR. Impact of depression on risk of myocardial infarction, stroke and cardiovascular decease in patients with psoriasis: A Danish Nationwide written report. Acta Derm Venereol. 2016;96:218–21.
-
Zhu B, Cao C. Correlative research between stigma, social support and quality of life in patients with psoriasis. Chin Nurs Res. 2016;30:3639–42.
-
Pichaimuthu R, Ramaswamy P, Bikash Thousand, Joseph R. A measurement of the stigma among vitiligo and psoriasis patients in Republic of india. Indian J Dermatol Venereol Leprol. 2011;77:300–half dozen.
-
Norreslet LB, Ebbehoj NE, Ellekilde Bonde JP, Thomsen SF, Agner T. The impact of atopic dermatitis on work life - a systematic review. J Eur Acad Dermatol Venereol. 2018;32:23–38.
-
Kwak Y, Kim Y. Associations between prevalence of adult atopic dermatitis and occupational characteristics. Int J Nurs Pract. 2017;23:e12554. https://doi.org/10.1111/ijn.12554.
-
Cazzaniga S, Ballmer-Weber BK, Grani N, Leap P, Bircher A, Anliker M, et al. Medical, psychological and socio-economic implications of chronic manus eczema: a cross-sectional report. J Eur Acad Dermatol Venereol. 2016;30:628–37.
-
Mattila Grand, Leino Thou, Mustonen A, Koulu 50, Tuominen R. Influence of psoriasis on work. Eur J Dermatol. 2013;23(2):208–xi.
-
Levy AR, Davie AM, Brazier NC, et al. Economic burden of moderate to astringent plaque psoriasis in Canada. Int J Dermatol. 2012;51:1432–40.
-
Itakura A, Tani Y, Kaneko N, Hide Chiliad. Bear upon of chronic urticaria on quality of life and work in Nippon: results of a real-world study. J Dermatol. 2018;45:963–70.
-
Schmitt J, Küster D. Correlation betwixt dermatology life quality alphabetize (DLQI) scores and piece of work limitations questionnaire (WLQ) allows the calculation of percent work productivity loss in patients with psoriasis. Arch Dermatol Res. 2015;307(5):451–iii.
-
Nguyen CM, Beroukhim K, Danesh MJ, Babikian A, Koo J, Leon A. The psychosocial impact of acne, vitiligo, and psoriasis: a review. Clin Cosmet Investig Dermatol. 2016;9:383–92.
-
Rzepecki AK, McLellan BN, Elbuluk N. Beyond traditional treatment: the importance of psychosocial therapy in Vitiligo. J Drugs Dermatol. 2018;17(6):688–91.
-
Paul D, Kinsella L, Walsh O, Sweenry C, Timoney I, Lynch M, et al. Mindfulness-based interventions for psoriasis: A randomized controlled trial. Mindfulness. 2018;10(2):288–300.
-
Hashimoto One thousand, Ogawa Y, Takeshima North, Furukawa TA. Psychological and educational interventions for atopic dermatitis in adults: A systematic review and meta-analysis. Behav Chang. 2017;34:48–65.
-
Van Beugen South, Ferwerda Thousand, Spillekom-van Koulil S, Smit JV, Zeeuwen-Franssen ME, Kroft EB, et al. Tailored therapist-guided net-based cognitive behavioral treatment for psoriasis: A randomized controlled trial. Psychother Psychosom. 2016;85:297–307.
-
Shah R, Hunt J, Webb TL, Thompson AR. Starting to develop self-help for social feet associated with vitiligo: using clinical significance to measure the potential effectiveness of enhanced psychological self-help. Br J Dermatol. 2014;171:332–vii.
-
Bundy C, Pinder B, Bucci Due south, Reeves D, Griffiths CE, Tarrier N. A novel, web-based, psychological intervention for people with psoriasis: the electronic targeted intervention for psoriasis (eTIPs) written report. Br J Dermatol. 2013;169:329–36.
-
Zill JM, Christalle E, Tillenburg North, Mrowietz U, Augustin M, Härter 1000, Dirmaier J. Furnishings of psychosocial interventions on patient-reported outcomes in patients with psoriasis: a systematic review and meta-analysis. Br J Dermatol. 2018.
-
Nagarajan P, Thappa DM. Event of an educational and psychological intervention on knowledge and quality of life among patients with psoriasis. Indian Dermatol Online J. 2018;9(1):27–32.
-
Heratizadeh A, Werfel T, Wollenberg A, Abraham S, Plank-Habibi Due south, Schnopp C, et al. Effects of structured patient pedagogy in adults with atopic dermatitis: multicenter randomized controlled trial. J Allergy Clin Immunol. 2017;140:845–53.
-
Jha A, Mehta Chiliad, Khaitan BK, Sharma VK, Ramam Yard. Cognitive behavior therapy for psychosocial stress in vitiligo. Indian J Dermatol Venereol Leprol. 2016;82(iii):308–10.
-
Keyworth C, Nelson PA, Bundy C, Pye SR, Griffiths CEM, Cordingley 50. Does message framing touch on changes in behavioural intentions in people with psoriasis? A randomized exploratory report examining wellness risk communication. Psychol Health Med. 2018;23:763–78.
-
Ahmed A, Steed L, Burden-Teh Eastward, Shah R, Sanyal S, Tour Due south, Dowey Due south, Whitton One thousand, Batchelor JM, Bewley AP. Identifying primal components for a psychological intervention for people with vitiligo - a quantitative and qualitative report in the U.k. using web-based questionnaires of people with vitiligo and healthcare professionals. J Eur Acad Dermatol Venereol. 2018;32:2275–83.
-
Ormerod E, Bale T, Stone Due north. Psoriasis direct service: an audit and review. Dermatol Nurs. 2017;xvi(1):45–ix.
-
Gionfriddo MR, Pulk RA, Sahni DR, Vijayanagar SG, Chronowski JJ, Jones LK, et al. ProvenCare-psoriasis: A illness management model to optimize care. Dermatol Online J. 2018;24:3.
Funding
This work was supported by Nursing Branch of China Research Hospital (NBCRH), which provided financial support during the search and screening of the literatures.
Author data
Affiliations
Contributions
XJZ and APW designed the research protocol, performed and analyzed the inquiry. XJZ and LF performed the search. Where questions arose, TYS, JZ and HX advised on article inclusion. TYS and JZ designed and tested the extraction forms. XJZ and APW designed the Tables. XJZ wrote the manuscript. XJZ, APW, TYS, JZ, HX and DQW read and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ideals declarations
Ethics approving and consent to participate
We strictly followed the standards of scoping review. There were no human participants and therefore no ethical approvals were not required.
Consent for publication
Not applicative.
Competing interests
The authors declare they have no competing interests.
Additional information
Publisher's Notation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is distributed under the terms of the Artistic Eatables Attribution four.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted apply, distribution, and reproduction in whatever medium, provided you give advisable credit to the original author(s) and the source, provide a link to the Creative Commons license, and signal if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this commodity, unless otherwise stated.
Reprints and Permissions
About this article
Cite this commodity
Zhang, Xj., Wang, Ap., Shi, Ty. et al. The psychosocial accommodation of patients with skin disease: a scoping review. BMC Public Health 19, 1404 (2019). https://doi.org/10.1186/s12889-019-7775-0
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12889-019-7775-0
Keywords
- Skin disease
- Psychosocial
- Adaptation
- Factors
- Scoping review
What Is Ta Similar Dermatological Skin Disease Related To Dhoenbergs?,
Source: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7775-0
Posted by: vinsonarmet1952.blogspot.com


0 Response to "What Is Ta Similar Dermatological Skin Disease Related To Dhoenbergs?"
Post a Comment